ID Card
Medicare Advantage
Policy Number: MA-X-002
Last Updated: Dec. 12, 2024
Our member identification cards contain basic information you will need when providing covered services to our members. The Blue Cross and Blue Shield of Nebraska (BCBSNE) Medicare Advantage ID card indicates the member is enrolled in a BCBSNE Medicare Advantage plan. Our BCBSNE Medicare Advantage members only need to show our ID card to receive services. A member doesn’t need to show their Original Medicare ID card to obtain services.
All Blue Cross Blue Shield Association (the national organization for all Blue plans) cards have a similar look and feel, which promotes nationwide ease of use. The cards include a magnetic strip on the back to provide easier access to eligibility and benefit information.
Providers must include the three-character alpha prefix found on the member’s ID card when submitting paper and electronic claims. The alpha prefix helps facilitate prompt payment and is used to identify and correctly route claims and confirm member coverage. It is critical for the electronic routing of specific transactions to the appropriate Blue Cross Blue Shield plan.
Below is a sample of the members’ ID card.
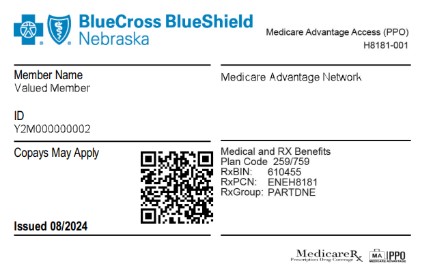
- YMA4 will be the new prefix for the HMO product
- Y2M4 will be the new prefix for the PPO product
The Medicare Advantage plans all have coverage outside of the service area for providers that accept Medicare Advantage (does not require Blue Card providers). As with other BCBSNE products, members should provide their ID cards when requesting services from you.
The front of the card may include:
- The Enrollee name, also called the subscriber or member, who is the contract holder.
- The Enrollee ID also called the contract number, which is made up of randomly chosen characters, either alpha-numeric or all numeric.
- The issuer ID number just below the member information. This number identifies which Blue plan issued the card (BCBSNE or another plan.)
- A logo in the lower right corner of many cards identifies the member’s prescription drug claims processor (for use by pharmacists).
The back of the card may include:
- Our website address
- A magnetic strip at the top
- Phone numbers
- An address showing where to send claim

